Making friends and finding social opportunities can sometimes be difficult, particularly for children with neurodevelopmental disabilities, such as autism spectrum disorder, attention deficit hyperactivity disorder, or an intellectual disability. Here’s what parents can do to help.
Building inclusive communities
Friendships and social connections are an important aspect of our lives. They provide a sense of belonging and allow people to be included in their communities.
People with neurodevelopmental disabilities may communicate, learn, and behave differently. Sometimes these differences make it harder than usual to develop friendships and participate in social activities.
But parents and others can help create more inclusive communities and opportunities to build social relationships, especially for people with neurodiverse abilities.
Below are some tips and strategies to help children learn and develop the social and emotional skills they need to make friends.
Practice at home: Tips for common social situations
Navigating social settings and making friends involve many skills you can practice with children at home.
- Greetings and questions. Make a habit of practicing greetings throughout the day. Model good listening for your child, and take turns asking and answering conversation starters like, “How are you?”
- Calm body movements. Sometimes it can be hard for children with neurodevelopmental disabilities to keep a calm body. Have your child practice giving their body enough room and keeping personal space between themselves and others by using an arm’s-length distance.
- Appropriate level of voice. Encourage your child to listen and match the level of your voice. Imagine your voice has a volume dial and practice turning the volume up and down.
- Eye contact. Looking directly into someone’s eyes can be difficult, so help your child instead look at different parts of your face or practice looking at their own eyes in the mirror.
- Reading and responding to social signals. People regularly communicate using more than just words. Social signals are the variety of ways in which we communicate through body language and facial expressions. Often this can be tricky to detect for children who are neurodiverse. Help your child recognize common social signals by asking what someone’s body or face might be saying.
Rerouting challenging behaviors to help children build friendships
Challenging behaviors may get in the way of making and keeping friends. It is important to address challenging behaviors like impulsivity and aggression through therapies and programming. Additionally, practicing the following fundamental skills can help reduce challenging behaviors.
- Patience. Learning how to wait for a turn to play or a time to speak in a conversation is an important social skill. Practice waiting with a timer, gradually building up from 10 seconds, to one minute, to five minutes.
- Flexibility. Help your child make compromises using first/then statements, such as, “First we play your way, then my way.” Model flexible play and redirect with new toys to show how play can evolve.
- Communicating strong emotions.Handling strong feelings can be difficult sometimes. Practice communicating these feelings effectively either by asking for help, using an emotions board, or taking a break.
How to throw a wide net socially
Encouraging social opportunities is an important part of supporting friendships and social relationships for children with neurodevelopmental disabilities. Social spaces offer chances for children who are neurodiverse to find activities they enjoy. They are able to practice the social and emotional skills they are learning and even meet other children practicing these same skills.
- Structure and organize play dates. Set up the environment before a play date by making a list of activities to do with a friend, then picking out of a hat which activities to do and in what order.
- Make a list of things that are fun to do and invite others to join. Look for free or low-cost programs or events out in the community.
- Connect with other parents of children with disabilities. Set up an activity for your children like an ice cream date, going on a walk, or a game night with adults and kids together. These encounters can give rise to repeat, planned social interactions.
- Check out organizations in the community for children with disabilities, like Special Olympics, or recreational programs that foster inclusive environments through Unified Sports.
- Look into facilitated recreational activities like a Lego club or pizza parties with teachers. Plan to bring a support person if needed.
Your child’s doctor or teacher may be able to suggest additional community or web-based resources designed to help families support friendships for children with neurodiverse abilities.
About the Authors

Sydney Reynders, ScB, Contributor
Sydney Reynders, ScB, is a clinical research coordinator in the Boston Children’s Hospital Down Syndrome Program. She assists in research investigating educational, behavioral, and medical interventions in Down syndrome and other neurodevelopmental disorders. She received her … See Full Bio View all posts by Sydney Reynders, ScB 
Nicole Baumer, MD, MEd, Contributor
Nicole Baumer, MD, MEd is a child neurologist/neurodevelopmental disabilities specialist at Boston Children's Hospital, and an instructor in neurology at Harvard Medical School. Dr. Baumer is director of the Boston Children's Hospital Down Syndrome Program. She … See Full Bio View all posts by Nicole Baumer, MD, MEd




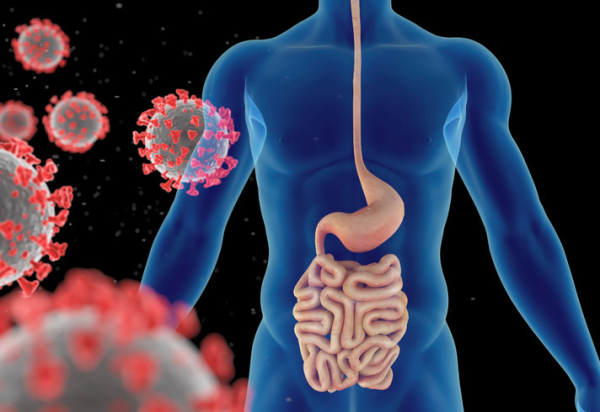
 Low energy, brain fog, and lung problems are a few of the lingering aftereffects reported by some people who have had COVID-19. Could gut troubles also fall among the constellation of chronic symptoms that people with long-haul COVID experience? And if so, what do experts suggest to help ease this?
Low energy, brain fog, and lung problems are a few of the lingering aftereffects reported by some people who have had COVID-19. Could gut troubles also fall among the constellation of chronic symptoms that people with long-haul COVID experience? And if so, what do experts suggest to help ease this?







 In today’s fast-paced world, our waking hours are filled with decisions — often surrounding what to eat. After a long day, dinner could well be fast food or takeout. While you may worry about the toll food choices take on your waistline or blood pressure, as a liver specialist, I also want to put fatty liver disease on your radar.
In today’s fast-paced world, our waking hours are filled with decisions — often surrounding what to eat. After a long day, dinner could well be fast food or takeout. While you may worry about the toll food choices take on your waistline or blood pressure, as a liver specialist, I also want to put fatty liver disease on your radar.